Less than a week after the Oregon Health Authority (OHA) declared an hMPXV, or Monkeypox, outbreak in Oregon, state health experts have recorded 95 confirmed or presumed Monkeypox cases across seven Oregon counties.
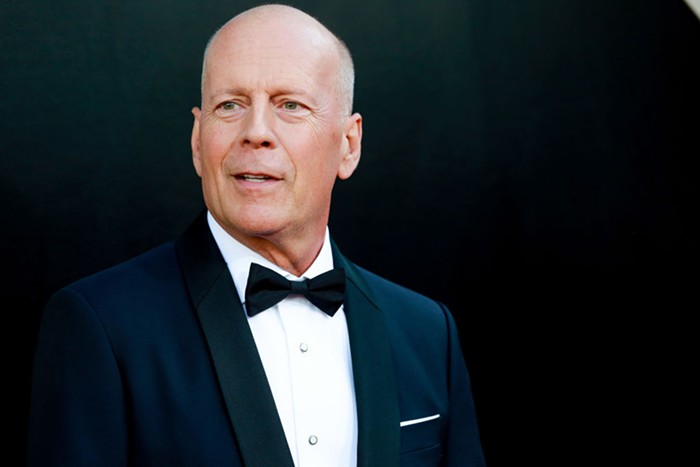
“Right now, the best thing you can do is to know your body and know the symptoms,” said state epidemiologist Dean Sidelinger during a press conference Thursday.
Monkeypox is a disease in the Smallpox family that transmits through prolonged skin-to-skin contact, most likely during sex. The disease can first appear as a rash or small pimples, which can then turn into larger, more painful lesions and wounds. The illness is not fatal, but can be very painful and create complex wounds that can be reinfected with staph or other bacterial infections, as well as leave scarring. Currently, a majority of the cases in Oregon and nationwide are amongst gay and bisexual men, but cases are expected to—and have already started—spreading to other communities, particularly in cities with larger outbreaks like New York City and Los Angeles.
Multnomah County has the largest concentration of cases in Oregon, reporting 57 presumed cases as of Thursday.
During a press conference Thursday, health officials stressed the importance of knowing how to lower your risk for contracting Monkeypox, not letting stigma interfere with public education, and getting vaccinated if you engage in high risk behavior.
According to Sidelinger, Monkeypox is not an easy disease to catch compared to COVID-19. The most common form of transmission is prolonged skin-to-skin contact with an infected person, especially contact with a rash, scab, or body fluids. While much less common, Monkeypox can also be spread by touching objects, fabrics, or surfaces that have been used by someone who is infected.
Because of the way the disease is spread, health authorities are advising people to be aware of their own bodies and check themselves for new rashes and pimples, particularly near their genitals and anus. Local, state, and federal health officials are also recommending people ask any sexual partners about whether they have felt sick or noticed new rashes, and consider limiting their number of sexual partners until they can receive a vaccine against Monkeypox.
Vaccines against the disease are available, but in short supply. So far, the OHA has received 6,803 doses of the Monkeypox vaccine, which is the same vaccine used for Smallpox. Of those doses, at least 2,187 have already been administered. OHA has 35 doses of the vaccine in storage and all other doses have been sent throughout the state to various county health departments and other vaccination partners. OHA is ordering additional vaccine supply, but orders are restricted due to demand throughout the US. The vaccine production, based in Denmark, is currently ramping up, but has yet to meet demand.
Vaccinations in Multnomah County are currently being prioritized for people who have had contact with someone infected with Monkeypox in the past 14 days, and people that the county has identified as high-risk based off of HIV records. Anyone who notices a possible symptom of Monkeypox or believes they may have been in contact with an infected person should contact their doctor or call 211, the Multnomah County hotline, to be connected with the appropriate public health resource.
In addition to prioritizing most at-risk groups, OHA is emphasizing disseminating public education about Monkeypox in Spanish. In Oregon, 28.4 percent of presumed cases are amongst Hispanic or Latino people, despite Hispanic people only making up 14 percent of Oregon’s population. Sideinger said OHA is also specifically partnering with community organizations that serve Latino Oregonians to announce vaccine opportunities.
While the inception of the outbreak has mostly affected men who have sex with men, health officials say everyone should be aware of the signs and symptoms of Monkeypox.
“Anyone who has skin is susceptible to this virus,” Katie Cox, executive director of queer and trans health organization The Equi Institute, said. “I’m hearing straight people say they don’t have to worry about it because it doesn’t affect them. At this point, it is not an if, but a when it will start affecting other communities.”
Cox said that blanket messaging towards gay men is a disservice to public health efforts, noting that people who have sex with multiple people through dating apps, people who attend raves and festivals, polyamorous people, or anyone who participated in the recent World Naked Bike Ride should all be paying attention to public health guidance around Monkeypox.
Anyone who contracts Monkeypox should isolate themselves until the lesions scab over and fall off, which could take anywhere from two to four weeks. Unlike with COVID, there is no dedicated federal funding to support people who have to take time off of work or need assistance with childcare during their isolation. Sidelinger said OHA is working with community organizations to try to provide financial assistance and support on a case by case basis.
“The lack of urgency from the federal government is concerning,” Cox said of the dearth of financial support. “Would that urgency look any different if it wasn’t impacting a historically marginalized community? Did we learn nothing from the AIDs epidemic?”
With a new school year approaching, Sidelinger said OHA is having conversations with the Oregon Department of Education (ODE) about potential areas of concern. While all Monkeypox cases in the state are currently among adults, there is still possible risk of caregivers passing the disease to a child or sexually active teens contracting the disease. Sidelinger said that transmission within schools isn’t a primary area of concern, but ODE may create guidelines for high contact sports, like wrestling.
“Right now, parents should not have Monkeypox at the top of their list of concerns for going back to school,” Sidelinger said. “School is a very low-risk setting for the transmission of Monkeypox.”
The latest information on Monkeypox in Oregon, including cases and vaccination efforts, will be posted on OHA’s new Monkeypox website.